
The Secret to Improving Your National & CAHPS Scores
Hospitals and healthcare providers often struggle in attempting to elevate national and CAHPS scores because of two main factors:
1. External
The primary reason why many cannot improve their CAHPS scores is attributed to the method employed to collect data. Traditional post-visit surveying methods (e.g. mail/phone) do not provide consistently high response rates in order to obtain a fundamental understanding of process execution and individual performance in a timely manner. This is reflected by low survey response rates, surveys not providing high-quality data, data taking days, weeks, and months to get reported, and very simplistic reporting tools.
2. Internal
Medical leaders often misunderstand the mechanics of CAHPS scores and, therefore, lack understanding on how to properly analyze data intelligence and how it can be improved. They are often out of the habit of effectively analyzing data, which, in turn, means they cannot apply better understanding to improvement actions.
Ultimately, many medical leaders get "stuck in the ditch" and have no means of being able to pull themselves out. Yet many still keep employing the same methods, hoping to get a different result which ultimately never comes.
CMS and Others Agree
This problem hasn't gone unnoticed, here's what CMS and others say about only depending on traditional methods of surveying.
"CMS emphasizes that HCAHPS scores are designed and intended for use at the hospital level for the comparison of hospitals to each other. CMS does not review or endorse the use of HCAHPS scores for comparisons within hospitals, such as comparison of HCAHPS scores associated with a particular ward, floor, individual staff member, to others. Such comparisons are unreliable unless large sample sizes are collected at the ward, floor, or individual staff member level . . .HCAHPS is not appropriate for comparing or assessing individual hospital staff members. Using HCAHPS scores to compare or assess individual staff members is inappropriate and is strongly discouraged by CMS."
- Centers for Medicare & Medicaid Services HCAHPS Quality Assurance Guideline V11.0, March 2018.
"No one wants to complete an 80-question survey via mail or any other mode, for that matter. That is why traditional means of collecting feedback from patients and residents yield small and out-of-date samples that often fails to deliver the understanding needed for physicians and staff to engage and improve."
- NRC Health (NRChealth.com), February, 2019.
Here's the Secret
To improve and attain superior CAHPS scores requires a scientific approach, a method which can be replicated to produce desired results. The scientific approach is illustrated by the following simple model incorporating the Internal/External analysis:
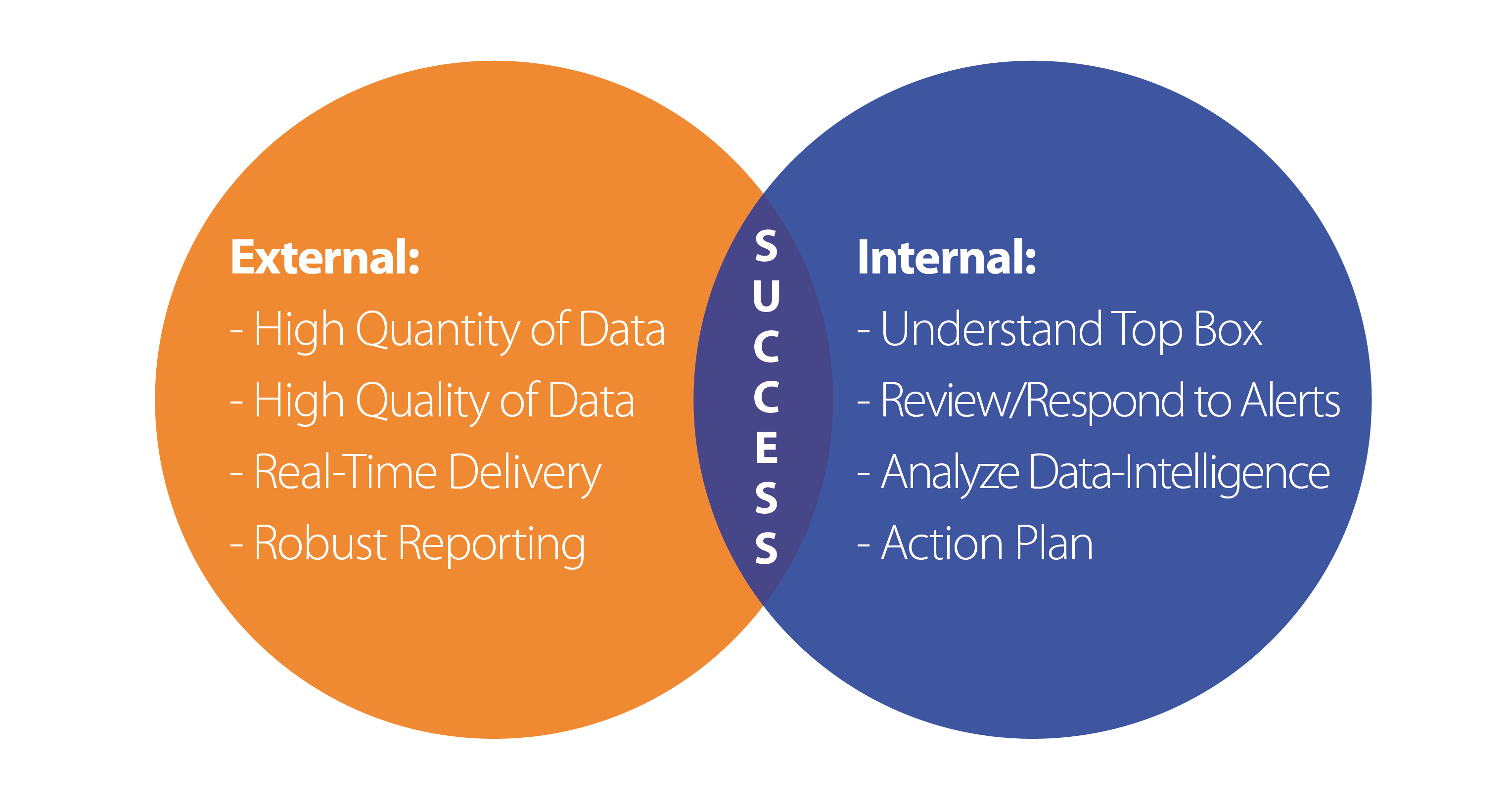
The model illustrated above reflects the symbiotic relationship between the external methods of data-collection/reporting and the internal work required to understand and apply for improved results. Success can only be attained when both are working in unison in a continuous loop.
Data-Collection and Reporting
Has to provide high quantity and quality of data. The data must be timely (i.e., real-time) and the reporting of data-intelligence has to be robust such that it fosters superior understanding of processes and execution by staff. This is the primary reason why many many cannot elevate their CAHPS scores. Hospitals often rely only on the CMS mandated mail/phone surveys, which do not provide any of these necessary attributes.
Internal Analysis and Application
Having all the necessary data in your possession is not enough; it has to be understood and then correctly applied. It's critical that medical providers understand the mechanics of CAHPS scoring (i.e., Top Box), as its improvement in this score which elevates national standing. Medical leaders should be responsive to survey alerts, thoroughly analyze data-intelligence, and then apply this improved understanding by formulating strategies and tactics in order to improve process and execution.
This scientific process of measurement, analysis, and application, using the correct tools is a proven method for success.
